My most challenging glaucoma case from last year
Glaucoma is a “whole of life” condition, and it’s reassuring that most people will have good vision and be able to continue working and pursuing their hobbies with
- good care,
- timely appointments and testing, and
- good compliance with the prescribed treatment.
However, there are patients for whom the diagnosis of glaucoma comes very late if they haven’t had regular eye checks or in whom the disease is very aggressive. You can’t tell if your glaucoma is getting worse just by judging how good your vision is.
2017’s most challenging glaucoma case
My most challenging glaucoma case from last year involved someone who had not been to see the optician for more than 20 years. Only when they had to start using reading glasses and had blurred vision in one eye did they have a routine eye check.
The patient had a family history of glaucoma. They had not concerned themselves about it and, like many of us, they were too busy to find a convenient time to have the recommended eye checks.
The optician’s examination revealed that their eye pressures were very high in both eyes. One eye had lost most of the vision already. In their mid-fifties and needing to drive for their livelihood, you can imagine how shocked and upset the patient was on hearing this.
At the first consultation, the testing and examination seemed very daunting to this patient, and they needed a lot of encouragement to complete the tests.
They were scared that the tests would show that theirs was a hopeless situation and nothing could be done
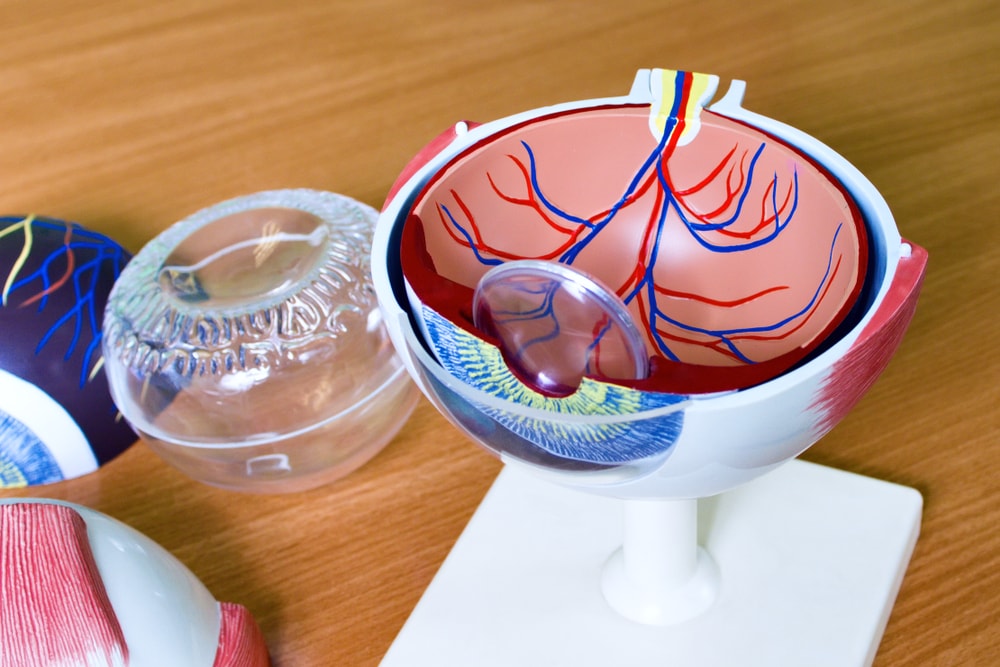
It is beneficial to be able to show patients the scans of the optic nerves at the back of the eyes. Furthermore, the visual field tests help to explain what damage glaucoma has caused and how treatment may save the vision they have left.
Alas, it is not possible to restore vision that is lost. In this case, the patient found that very hard to accept. He could only just see the top letter on the chart with the left eye. He had lost all but a small window of the central visual field in this eye. The right eye could still see most of the letters on the chart, but there was an early defect in the top part of the visual field.
Unless I could urgently control the pressure, this patient was at high risk of permanently losing the vision in this eye as a young working-age person with a family to support. He was the only driver in this family and could not do their job at the time without a driving license that allowed them to drive passengers around.
As so often happens when I see patients like this for the first time, it seems like a hopeless situation, and there is considerable grief and frustration.
There is also anger and regret at not having made the time for the checkups earlier and fear about the future and not being able to work or drive.
Denial is also typical -“ I can see well in the good eye”, and there is an initial reluctance to take treatment. There is often resistance to taking medication due to perceived side effects. All of these were true in this case and the denial extended to this person carrying on driving passengers around when they did not meet the driving standard for this.
It is so important to have a good two-way relationship between patient and glaucoma specialist in these cases.
As a patient, you have to trust your specialist and feel able to ask questions. You want to feel comfortable to ask them to explain things again if you haven’t understood.
How family members can provide crucial support towards an optimal outcome in a challenging glaucoma case

In this case, the patient and I had a good relationship, and they ceased driving passengers around immediately when I explained that they were no longer safe or legally allowed to do so. Their adult son, however, found this more difficult to accept and was initially abrupt and questioning in consultations.
They had come to support their parent. It is hugely important for your family and friends to support you through glaucoma surgery. It is not uncommon for them to be “outraged” or angry on your behalf when someone tells you that you have glaucoma and treatment is for life through no fault of your own. However, a united approach is necessary to achieve the best outcome for you. That often means, as in this case, persuading the family members that surgery is entirely the right thing to do and that the risks of doing nothing are not zero!
In this case, one of the main difficulties was assuring the son that not operating was much riskier than the procedure itself. I find it crucial to build relationships with the patients’ support network. In some cases, that means a consultation takes twice as long, or we might need to pause things to allow for a family discussion. Sometimes a second consultation is necessary to make sure that the patient has the support of their loved ones in the choice that they make.
What I needed to do was perform surgery on both eyes because drops alone – in the long-term – were not going to be enough to control the pressure

Having any operation is difficult. Whilst my patient was accepting of it for the left eye, the worse of the two, the prospect of having surgery to the good eye (and arguably the eye that needed the operation more to save their sight) absolutely terrified them. In such cases, I always try to stabilise the pressure in both eyes with maximum drops and tablets so that I can operate on the worse eye first.
It is essential to have someone go through trabeculectomy surgery in the eye with less vision first; to feel what it is like and to understand that recovery takes weeks, not days. The vision is almost always more blurred in the first few weeks after the operation. It improves day-by-day to the level it was before surgery. The patient must appreciate that the four visits in the first six weeks after the operation are critical to the success of the operation. They must understand why they cannot miss or delay an appointment without potentially affecting the outcome of surgery.
The first operation went well, and the plan was to do the same thing on the “good” right eye. Can you imagine going to sleep for an operation, waking up with your good eye bandaged up, and then having to rely on your weaker eye for the first few weeks; an eye that can only just see the first letter on the vision chart?
I am a highly skilled surgeon who has carried out many of these operations in very precious ‘only eyes’ and in the trickiest of glaucoma situations. The surgery itself – and its challenges – are something I have done extensive training in to perfect my technique and get excellent results.
It was the initial building of the relationship with my patient’s son that made all the difference to the success in this case

He was there to encourage his parent in the initial days after surgery when they needed help to get around and do the basics in life we all take for granted. He could help with day-to-day tasks such as eating, dressing and moving from the bedroom to the kitchen. He could help them stick to the drop schedule and encourage them to accept that day-to-day they were getting better.
Three months after surgery to the second eye my patient was off all drops, with good pressure control and back to work with the same company in a role that didn’t require them to transport passengers.
They had confirmation from the DVLA that they could drive a normal car for leisure. Apart from now making time to have the necessary glaucoma eye checks, they are carrying on as before. My patient knows they will need cataract surgery to both eyes in due course. We must once again face operating on the “good eye”, as well as the weaker one.
They are most thrilled about the fact that their adult children, including their son who was initially so resistant to any treatment, are now having regular eyes tests so that if they too develop glaucoma, it can be picked up and treated early. They frequently spread the word to their work colleagues and friends about the importance of routine eye testing.
This most challenging glaucoma case sticks in my memory
It started out with high levels of grief and anxiety about a late diagnosis involving not just the patient but their family too. It ended up not only with a good result for the patient but the wider positive benefits of the awareness of glaucoma and how a good patient support network is needed. This network includes me as the glaucoma specialist, my specialist nursing team, and the International Glaucoma Association to whose website I direct patients for more information. Having such a support network enhances positive outcomes for patients and family allowing them to adapt their lives positively to live with glaucoma instead of ignoring glaucoma – which results in poorer outcomes.






Leave A Comment