What is Glaucoma?
Are there different types of glaucoma?
Ophthalmologists divide Glaucoma into different subtypes. The thing that they all have in common is that the optic nerve is damaged.

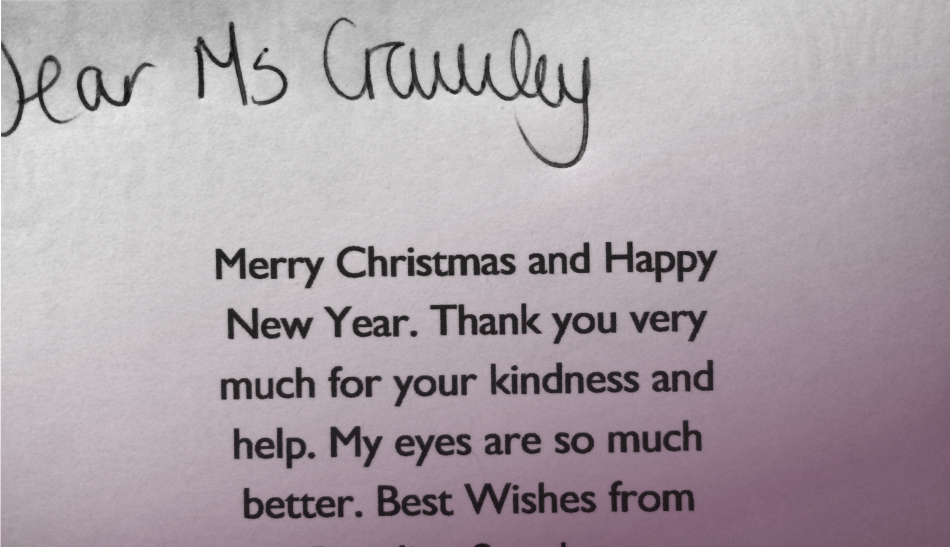
I had the best experience working with Dr Crawley. I felt looked after and she took the time to get to know me. I would highly recommend her.

From the moment I met her to the moment I left, I was treated with great courtesy and kindness, and everything was explained to me in layman’s terms so I could fully understand my condition. I was immensely impressed.

“Thank you very much for seeing me yesterday, you were marvellous and a pride to the NHS”

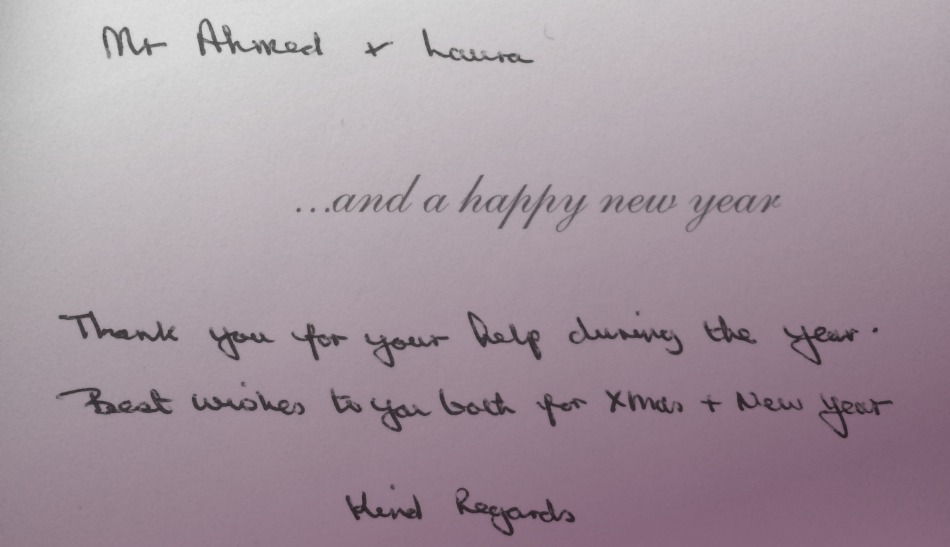
Dear Laura,
Just a quick note to say thanks for looking after my mum Mrs M. so wonderfully. It was so good of you to take so much time and care as she was very worried about my appointment and you really made such a difference to my experience. Thank you.

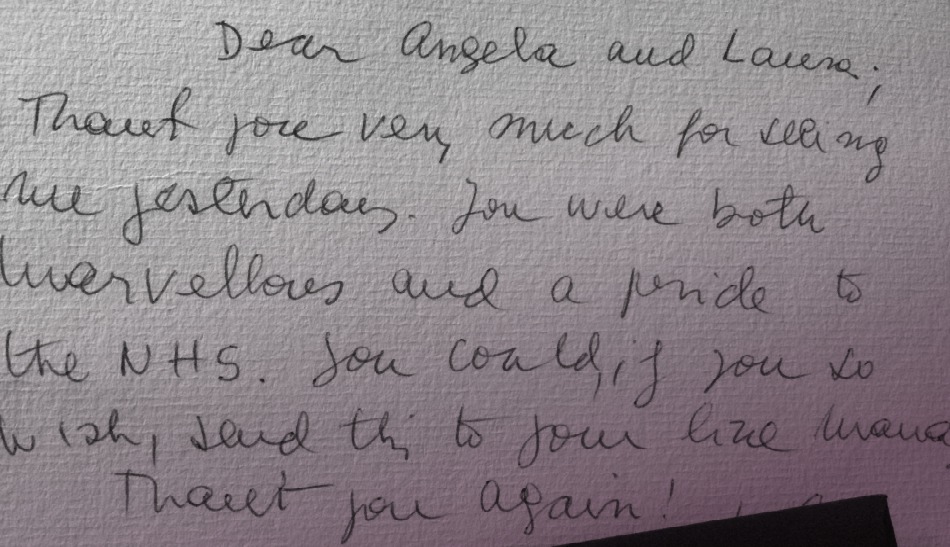
Dear Angela and Laura,
Thank you very much for seeing me yesterday. You were both marvellous and a pride to the NHS. You could, if you two wish, send this to your line manager. Thank you again!

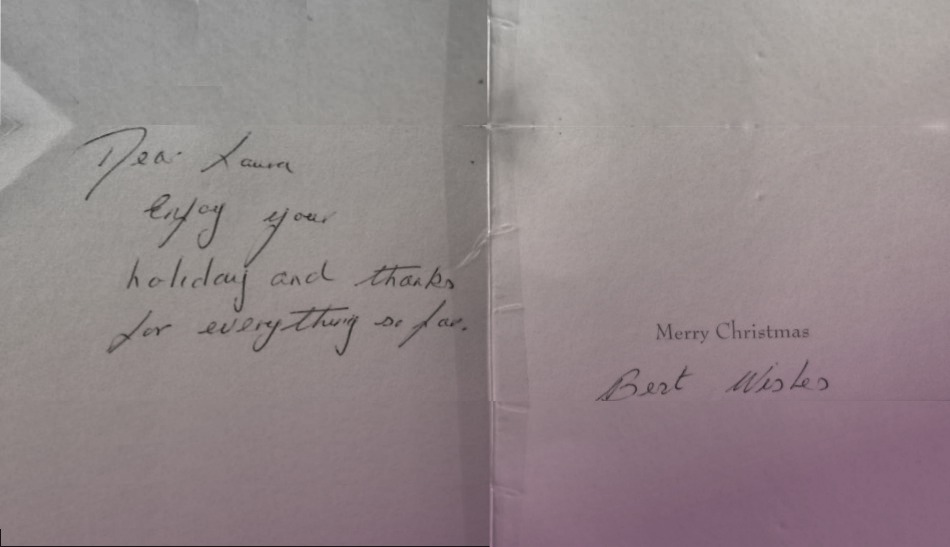
Dear Laura,
Enjoy your holiday and thanks for everything so far.
Best Wishes
Primary Open Angle Glaucoma
The most common type of glaucoma is Primary Open Angle Glaucoma (POAG). The IOP may be higher than normal (normal range 10-21mmHg) but not always. The patient has no symptoms. The specialist checks the eye pressures and finds them to be high. In another instance, the optician looks at the back of the eye and suspects that the optic nerve looks damaged in a particular pattern.
The human eyeball is a closed chamber which produces fluid (aqueous) and drains it away. This internal circulation of fluid within the eye is not the same as your tears. In POAG the drainage system does not filter the fluid for reasons we still do not understand. Some people have optic nerves that are more susceptible to damage. In these patients even normal IOP can cause damage to the nerve. The damage may be because the blood supply to these particular optic nerves doesn’t function.
It is also possible that the support for the optic nerve as it travels into the back of the eye is weak. However, we can not alter either of these factors. Reducing the IOP in POAG is the only treatment option at the moment. Even if the starting IOP is within the normal range.
Angle Closure Glaucoma
In some patients, the drainage channels that filter the aqueous within the eye are too small. One cause of this could be the fact that if people get older, we develop cataracts in their eyes. The evolving cataract can push against the drainage channels and make them smaller and narrower. In some cases, blocking them off altogether. This blockage causes the IOP to rise resulting in acute glaucoma. A situation like this is an ophthalmic emergency, requiring urgent eye pressure reduction, otherwise, it could lead to permanent loss of vision.
It is important that the glaucoma specialist examines the drainage angles correctly. If we see narrow drainage angles before an acute attack occurs, we can do a laser treatment to reduce the chances of an assault. This procedure called a ‘peripheral iridotomy.’ A peripheral iridotomy is a tiny hole in the iris, the coloured part of your eye. It is similar to the hole at the top of your sink that stops the sink from overflowing. Not a hole in the eye, more like an extra pupil at 12 o’clock in the iris. No one can see it, and it is positioned in a part of the iris that lies beneath the upper lid.
In some cases, laser alone does not allow enough space for fluid to drain. It may be necessary to remove the growing cataract to restore the space for aqueous fluid to drain. This means that we sometimes operate on cataracts for IOP rather than for vision.
Secondary Glaucoma
These are less common than POAG. In POAG we don’t yet know why the drainage channels stop working. In secondary glaucomas, there is a clear reason for the rise in IOP.
- Trauma.
- Rubeosis. Abnormal blood vessels grow inside the eye due to diabetes, blocked veins or arteries inside the eye, or poor blood supply in the carotid arteries in the neck. Rubeotic glaucoma is aggressive and almost always requires many surgical procedures.
- Pseudoexfoliation. Also known as PXF. Signs of PXF are white powdery deposits on the lens, iris and drainage channels inside the eye. It can be associated with high IOP and glaucoma that progresses fast. Early treatment and close follow-up are essential.
- Pigmentary glaucoma. Occurs when the iris rubs against the human lens that lies close behind it. This ‘rubbing’ dislodges the pigment that gives our eyes their colour. The pigment then clogs up the drainage channels leading to raised IOP and glaucoma. It mainly affects younger short -sighted people. Pigment shedding can often increase during exercise.
- Previous eye surgery. Previous retinal detachment surgery involving silicone oil enhances the risk of glaucoma.
- Inflammation. Patients who have chronic and repetitive inflammation in their eyes can develop glaucoma. This may be due to inflammatory related scarring of the drainage channels themselves. It also can be a response to the steroid drops that are necessary to treat inflammation.
In all cases of glaucoma an individualised glaucoma treatment plan is necessary and is based on real clinical evidence.
The best way to figure out your eye treatment options is to give us a call on: 02079357990,
or click below to request a call back:
Accreditations and Memberships
Related articles
My most challenging glaucoma case from last year
In this post, I share a story about my most challenging case of 2017. I had a patient who had not seen an optician for 20 years and discovered he had glaucoma. It's a story that exemplifies the importance of having a strong, supportive network to around the patient that can help them make good decisions and help them cope with the initial adjustments after the operation.
Humphrey visual field test
Humphrey visual field testing is a critical test for diagnosing and managing glaucoma or other causes of damage to the optic nerve.
Do I need cataract surgery?
In the past, a cataract did have to be “ripe” before surgery could be undertaken, but modern cataract surgery can be done at any time, and the decision to go ahead with surgery should be based on how the cataract affects you in your day to day life.























Find us on social media